Cervical myelopathy is spinal cord compression in the neck and mainly happens in those over 55 years of age. It is commonly pressure and damage to the anterior spinal cord from a disc herniation, bony spurs from Spondylosis or degeneration, spinal stenosis or an ossified posterior longitudinal ligament. If we consider the nervous system as a tree, with a trunk and branches, then Myelopathy is con-stricture of the trunk – the spinal cord – and radiculopathy is pressure on the branches – the nerve roots.
Early symptoms include weak, clumsy, painful hands, and lack of fine motor skills or finger dexterity. Walking with a clumsy or unsteady gait may happen. There may be no pain, or neck pain and stiffness may occur, with shoulder pain radiating into the arm.
It is a slowly progressive disorder, and can either be mild or severe, sometimes requiring surgery. It is diagnosed by clinical signs and symptoms, as well as an MRI scan. Complete remission to normal function is very rare. In mild cases, it can be treated with manipulation, Chiropractic and muscle releasing techniques (see below) which focus on relieving symptoms and preventing a deterioration of the compression where possible. Severe cases may require surgery to maintain the nervous function as best as possible, mainly also to prevent deterioration of symptoms.
Cervical Myelopathy Statistics
This is the most common spinal cord disorder in the over-55s.
90% of asymptomatic persons over 70 years have some degenerative change in the cervical spine.
Cervical spine myelopathy with narrowing and compression of the spinal canal occurs in 90% of us over 60 years old.
Both sexes are affected equally, but it tends to start earlier in men (50 years) than in women (60 years).
In 20% of cases, stenosis occurs in tandem in both the lumbar and cervical spine.
Causes of Cervical Myelopathy
The spinal cord compression commonly results from:
- Degenerative changes, like cervical spondylosis, or following trauma
- Disc degeneration
- Spinal stenosis
- Osteophyte formation at the level of facet joints
- A congenitally narrow spinal canal (<13mm) where there is less space
The neck is stabilised and protected by a group of ligaments. These ligaments can ossify, and this bone growth presses on the spinal cord:
- The posterior longitudinal ligament can be affected because it lies within the vertebral canal
- The Ligamentum Flavum (the “yellow ligament”) can cause progressive spinal cord and nerve root compression due to its hypertrophy, calcification or ossification.
Clinical symptoms of Myelopathy
Symptoms can vary, but there is often a slow, insidious onset with no trauma, commonly around the age of 50-60 years. Sometimes there is no pain, meaning the condition can be present for several years before symptoms appear.
Early symptoms include:
- Numb, clumsy, painful hands and loss of fine motor skills.
- Unsteady or clumsy gait
- Weakness and numbness occur in a non-specific/non-dermatomal pattern (whereas with cervical radiculopathy, pain follows a particular pattern)
As the spinal cord is compressed further, the weakness increases; muscle atrophy of the fingers can make fine finger movements difficult.
Musculo-skeletal symptoms of Myelopathy
- Neck pain and stiffness, especially in extension.
- Pain in the shoulder, arms, upper back and scapulae.
- Paraesthesia or numbness in one or both arms or hands with signs of radiculopathy.
Clinical signs
- Ataxia and dexterity loss.
- Hyper-reflexive patellar and achilles tendon reflexes.
- Presence of pathological reflexes – clonus, Babinski and Hoffman’s signs
- Spastic quadriplegia, sensory loss and bladder-bowel disturbance
- Increased reflexes in the lower extremities and in the upper extremities below the level of the lesion.
- Numbness and paraesthesia in one or both hands
Deterioration and Progression
Usually once the condition is diagnosed, a return to normal is unusual.
- 75% have episodes with neurological deterioration
- 20% experience a slow, steady progression
- 5% of cases present rapid onset and progression.
Nurick Classification of Cervical Myelopathy

| Grade | Symptoms |
|---|---|
| Grade 0 | Root symptoms (cervical radiculopathy) only, or normal |
| Grade 1 | Signs of cord compression; normal gait |
| Grade 2 | Gait difficulties, but employed or able to work |
| Grade 3 | Gait difficulties prevent working or employment, but can walk unassisted |
| Grade 4 | Unable to walk without assistance |
| Grade 5 | Wheelchair or bedbound based on gait and ambulatory function |
Structural, Vascular and Cellular Changes
With compression on the spinal cord, there is ischemia or reduced blood flow and oxygen to the spinal cord, which then affects the protective covering of the spinal cord and causes demyelination.
Demyelination
Myelin is an insulating material – the protective sheath of nerve cells around the spinal cord. It is similar to an electric cable with a plastic outer covering around the metal wires underneath. Myelin around the nerves allows the signals to transmit much faster along the nerve. When myelin is damaged, it can lead to neurological symptoms.
Myelin can be damaged through physical pressure, loss of oxygen, metabolic problems or infections. Symptoms of demyelination can include:
- Pain, numbness
- Loss of reflexes and uncoordinated movements
- Poorly controlled blood pressure
- Racing heart or palpitations
- Blurred vision
- Dizziness
- Memory problems
- Loss of bladder and bowel control
- Fatigue
Diagnosis of Cervical Myelopathy
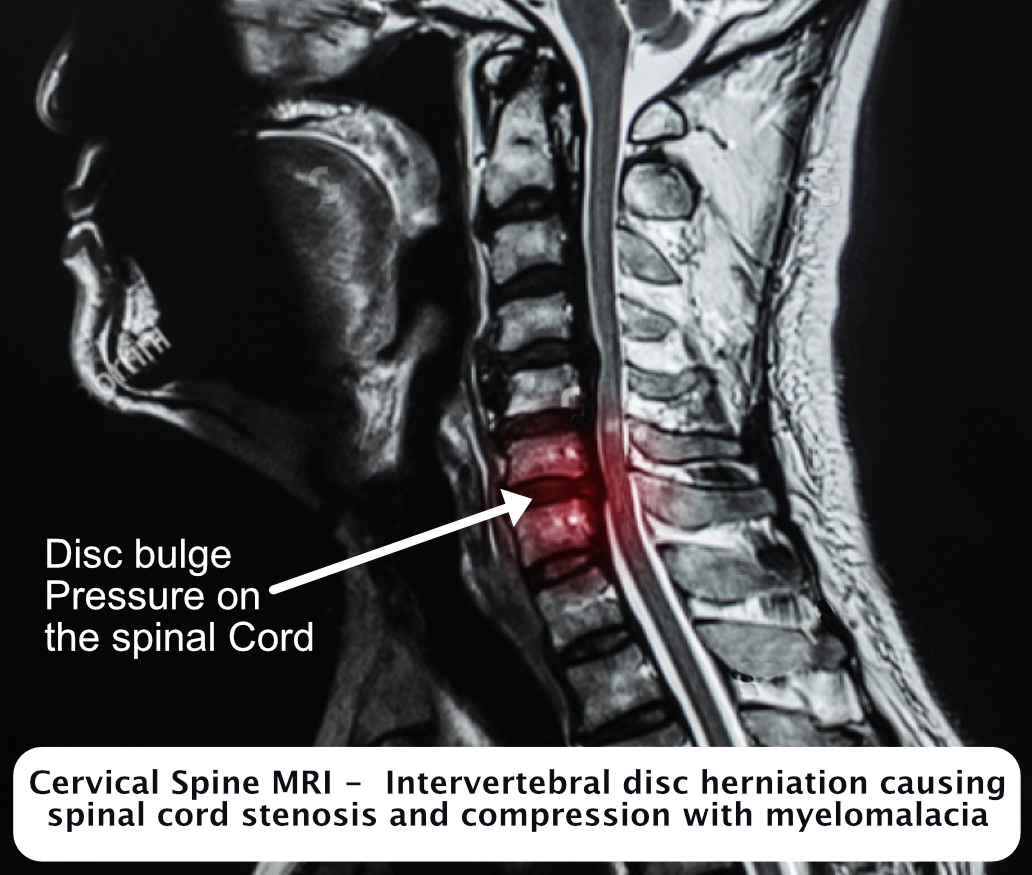
Neurological examination and history can give a good indication of the condition; however, MRI is the current gold standard to diagnose the degree and severity of cervical myelopathy, and will lead the treatment plan.
Benefits of MRI:
- Determines the degree of spinal cord compression
- Anterior-posterior width reduction can be measured
- Cross-sectional imaging of cord compression
- Shows obliteration of the subarachnoid space
- Signals intensity changes to the cord, confirming spinal myelopathy
- MRI findings can correlate with the physical examination findings
Differential Diagnosis
There are many other conditions that can give similar neurological symptoms to cervical myelopathy, many of which can be distinguished by the physical exam or the MRI findings. Cervical Radiculopathy, Cervical Sprain and Strain, Chronic Pain Syndrome, Diabetic Neuropathy, and Multiple Sclerosis Spinal Cord Injury are among some of those conditions.
Surgical treatment of Cervical Myelopathy
If there are progressive neurological symptoms of weakness, numbness or falling then a referral to a spinal or neurosurgeon is required. The main aim of surgery is to HALT the progression: to stop the symptoms deteriorating. The longer the cord is compressed, the less likely it is to recover, especially if symptoms have been there for over 18 months. Surgery may not necessarily improve the condition, but can help to stop the condition from deteriorating, so to preserve the current level of nerve functioning.
For cervical myelopathy surgery, the main aim is decompression of the spinal cord and to prevent a deterioration of symptoms. In the Cervical spine there is less space for the spinal cord in general, but surgery is often more effective at areas where there is a larger space available for the spinal cord. It’s estimated that out of 10 operations, 7 no different, one will be worse, and two better. But for the 7 who are no different, if it can halt the progression, the surgery has been successful.
Surgery is likely to be more successful in younger people with a shorter history of symptoms, where the compression is at one defined level, rather than at multiple levels. As with most medical treatment, early diagnosis and treatment may be the key to minimise postoperative degeneration.
Thank you to Bob Chatterjee, spinal consultant, for his information. www.harleystreetspine.co.uk
Conservative treatment of Cervical Myelopathy
There is no one perfect treatment for the mild and moderate cervical myelopathy. The aim is to help reduce pain and maintain joint movement and function as best as possible. Any treatment that can help slow the progression of the cord compression and help with quality of life needs to be considered. Some reports suggest that surgery for patients in this category is not always beneficial, both two and ten years later.
Main aims of treatment:
- Relieve pain
- To reduce spinal cord compression
- To improve function and mobility
- To prevent neurological deterioration
- To reverse or improve neurological deficits
Chiropractic Treatment of Myelopathy
Cervical traction and manipulation has been shown to help reduce the pain, improving the cervical range of movement and decreasing neck muscle spasm in milder forms of myelopathy, which can but only help with improving blood vascularity and reducing compression. It can give some improvement of weakness, headaches, and dizziness. If this can then help in any way to improve symptoms and quality of life and either improve function, or even simply prevent a deterioration of neurological symptoms, then it has value.
Manipulation is not going to help every case of cervical myelopathy, but can be hugely beneficial for those clients which it does help.
It is likely that clients who benefit from manipulation will require on-going maintenance treatments to maintain the cervical function as the aim of the treatment is not to fully cure the condition, but rather to manage the symptoms.
Some clients may not benefit or be suited to manipulation, however, deep muscle releasing and gentle traction to the suboccipital muscles can sometimes be extremely effective at helping movement, vascularisation, and reducing pain in the neck.
Exercises
Manipulation and exercise have been shown to be beneficial together, along with learning how to avoid strain and pressure on the neck.
Alexander Technique
Alexander Technique has several advantages in helping treatment of cervical myelopathy. It is very gentle, not placing strain on the cervical joints, and therefore may be more suited for some patients.
Because Alexander Technique focuses on releasing cervical muscular tension, improving and releasing the tension and awareness of the habitual patterns that create further stress and compression, it can help teach patients how to manage and look after their condition as best they can.
Alexander Technique is also aimed at helping maintaining good posture and workstation habits, that can directly lead to increased cervical tension. This is especially relevant as more of us are tending to get locked in one position and spending hours and hours sitting at the computer, or using phones and laptops in bad positions on the bed or sofa.
Chiropractic and conservative treatment both pre- and post-surgery
In surgical cases, there is still a place for more gentle Chiropractic treatments to help improve and restore cervical mobility, and reduce muscular spasm that may either have been long-standing or arisen from the surgery.
Other useful techniques and treatments include:
- Exercises to improve mobility and proprioception.
- Gentle mobilisation to help neck mobility.
- Gentle muscle releasing of the cervical muscles that are tight or in spasm.
- Improving the blood flow to the muscle in the neck, in term helping with blood flow to the deep tissue and promoting healing.
For more information, please visit www.physio-pedia.com/Cervical_Myelopathy.
