Explaining Sciatica
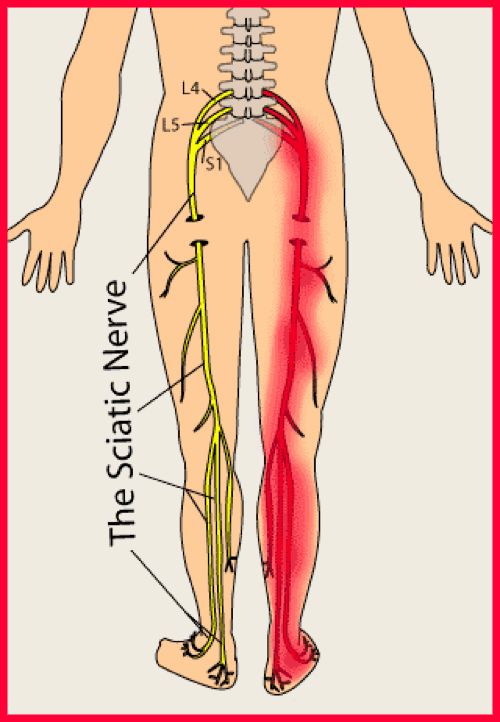
The sciatic nerve is the largest single nerve in the body and is composed of individual nerve roots that start by branching out from the spine in the lower back and run down the back of each leg. Portions of the sciatic nerve then branch out in each leg to innervate certain parts of the leg – e.g. the buttock, thigh, calf, foot, or toes.
Sciatica is pressure, irritation, inflammation or ‘pinching’ of the sciatic nerve which extends into the leg and the foot. The label of ‘sciatica’ is given out by the medical profession far too often when there are no clinical signs and the pain is in fact ‘referred pain’. Not all back pain with leg pain is sciatica. Chiropractors are well trained to help spot the difference between simple back pain (without nerve irritation) and sciatica.
Sciatic pain can vary from infrequent and irritating to constant and incapacitating. Specific sciatica symptoms also vary widely in type, location and severity, depending upon the condition causing the sciatica.
Chiropractic Treatment for Sciatica
Chiropractic adjustments to the spine help to free the locked movements in the facet joints in the spine, which helps release the pressure around the nerve canal, relaxing the small muscles that can be in spasm or restricting the space for the nerves to exit out of the spine.
Massage therapy may be used to reduce muscle spasm, and is also very effective. Massage can be applied either to the deep muscle in the lumbar spine, or for the inflammatory reactive muscle spots that can occur on the path of the nerve. Treatment helps the movement and blood circulation as well as reduced nerve pressure, which again allows the body to heal.
Sciatica symptoms
You can have any of the following:
- Back or buttock pain initially, which can continue, reduce or stop
- Pain in one leg – into the back of the leg, buttocks and commonly below the knee to the calf, either front or back
- Sharp pain, worse on sitting
- Coughing/sneezing can give spasms, or electric shock-like ‘jolts’ of pain in the leg
- Pain is usually just one side, sometimes alternates, but rarely both legs simultaneously
- Numbness, pins and needles, tingling or burning, which varies depending on which part of the nerve is affected
- Weakness of the foot and ankle, giving ‘foot-drop’ or limping
Clinical or neurological signs of sciatica
Along with symptoms above, there are clinical signs that your Chiropractor or doctor can test for:
- Numbness and loss of sensation in the toes or feet
- Straight leg ‘nerve-traction’ test is limited and increases the leg pain
- Weakness in the foot or toe muscles
- Lower limb reflex changes
Common Causes of Sciatica
Disc bulge or protrusion on the nerve
The commonest cause of Sciatica is protrusion of a disc that can impinge on a nerve.
Since the introduction of MRI scans, much has been learnt about disc protrusions or bulges, and we now understand that many healthy people, up to about 40% or higher, asymptomatic with no back pain or leg pain, can have some kind of disc pathology. However, only 4% of those people have actual compression on the nerve. The key is in maintaining disc health.
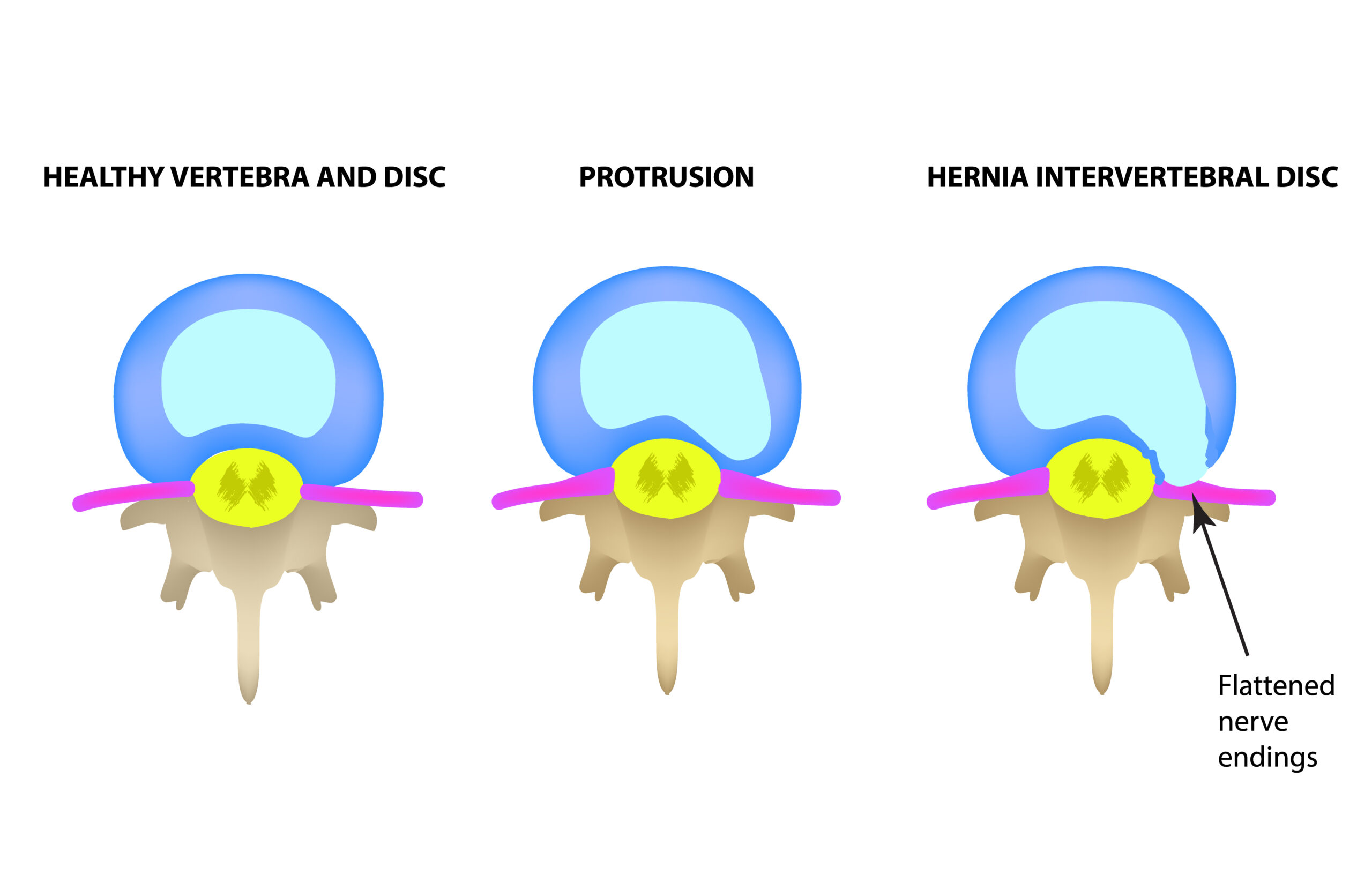
Types of disc bulges
There are various types of disc injury. Most of the time disc injuries, with simple tears to the cartilage – ‘Annular tears’ – can heal. It is when the disc ‘extrudes’ or ‘fragments’ that it can lead to more severe sciatica, as shown in the picture.
Commonly, the protruding part of the disc that shows on MRI scans is in fact inflammation, which can settle well with rest, time, exercise and treatment.
Spinal levels of disc involvement – L4/5 and L5/S1
The most common levels for the discs to herniate are at the lowest two disc levels, L4/5, pressing on the L5 nerve root and L5/S1 pressing on the S1 nerve root. They give slightly different symptoms and clinical pictures. Often it’s not easy to isolate which level is involved, and this will now be confirmed by MRI scans, but some typical signs are:
| L4/5 prolapse | L5/S1 prolapse |
|---|---|
| Straight leg raising reduced | Straight leg raising reduced |
| Ankle jerk present | Ankle reflex jerk absent |
| Weakness in toe and foot dorsiflexion (“foot-drop”) | Weakness in plantar flexion and foot eversion |
| Sensory loss – medial foot/big toe | Sensory loss – lateral foot |
| Pain down front of shin/lower leg | Pain down back of calf to foot |
Healing of Discs
The key to healing is allowing the body to keep a good blood supply to the disc, to help remove the debris and damaged discal material and create new cartilage fibres in the disc. The body has an amazing way of healing and the key is to allow the body to do its job. Sometimes a disc can take time to heal, and for full strength to return into a disc can take up to a couple of years, although the movement and much of its ability to function can return well before then.
It’s not always possible to prevent sciatica, and the condition may recur at the same level although it can sometimes reappear at a different level in the spine, giving different symptoms.
It’s most likely that once a disc has been injured that it will never be 100% as strong as previously, but most of the time they can heal sufficiently to allow us to carry on with our daily lives.
Piriformis syndrome
Another fairly common cause of sciatic nerve irritation and compression is from spasm or tightness in the piriformis, that lies above or around the sciatic nerve. Pain usually arises from the buttock, but can sometimes be very difficult to differentiate from a herniated disc. Commonly it settles more easily and quickly than a herniated disc. Please read my full article on Piriformis Syndrome for further information.
Pain and healing cycle in sciatica
Whilst there is usually variation on this, the pain and healing cycle in sciatica is commonly:
Back pain
↓
Leg pain – below the knee
↓
Foot weakness/numbness
↓
Back pain settles
↓
Lower leg pain settles
↓
Foot strengthens slowly – can take several months
↓
Numbness and sensation returns last (can be lengthy to settle in full)
Risk Factors for Sciatica
- Age – most common at 45-64 years
- Increased risk with being tall
- Mental stress
- Driving, including vibration of whole body
- Occupation – strenuous physical activity. A job that requires you to twist and bend your back, carry heavy loads or drive a motor vehicle for long periods might play a role in sciatica, but there's no conclusive evidence of this link.
- Prolonged sitting. People who sit for prolonged periods or have a sedentary lifestyle are more likely to develop sciatica than active people are.
- Diabetes - affects the way your body uses blood sugar, increases your risk of nerve complications.
- Smoking – weakens the discs probably through decreased circulation and blood supply.
- Obesity. By increasing the stress on your spine, excess body weight can contribute to the spinal changes that trigger sciatica.
Medical Treatment for Sciatica
Within the medical profession there are four or five basic options:
Rest – This will be advised if the condition is Acute or recent. You may be advised to take painkillers or anti-inflammatory drugs
Physiotherapy – exercises are commonly now given.
If the pain continues with Sciatic symptoms, referral to a specialist physiotherapist
MRI scan may be given
Possible referral to spinal surgeon
Cortisone or nerve block injections
Spinal surgery if symptoms indicate it and there is clearly no improvement or pain is too severe
My own view is that Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and injections should only be used if absolutely necessary, as they do not actually help the body and disc heal faster, but may actually inhibit and weaken the healing process, as I write about in ligament injury and healing.
Will I need surgery for my sciatica or disc bulge?
Commonly not! The medical profession now has studies that show surgery for sciatica is mostly not required, that the majority of cases will settle. Research showed that people who do NOT have surgery improve after two years to a similar extent to those who have surgery.
Surgery is now performed on an individual clinical basis, for those patients with severe disc bulges or extrusions that are giving constant and relentless pressure and pain or damage to the nerve root and that any more conservative care that can be given is worthwhile, including spinal manipulation.
‘Red flag’ or Danger Signs – When to See a Doctor
Although most people recover fully from sciatica, often without treatment, sciatica can occasionally cause permanent nerve damage. It can be very common with sciatica that sitting on the toilet is painful, and twisting even more so, but usually the bowel and bladder movements are normal.
Cauda Equina Syndrome is a very rare condition where there is loss of function or control with bowels and bladder. This is an immediate referral for medical care. Symptoms may include:
- Sphincter or gait disturbance
- Numbness around the bottom area - saddle anaesthesia
- Difficulty in going to the toilet (either bowels or bladder).
- Lack of bowel or bladder control
- Severe back pain usually in both legs.
With Cauda Equina symptoms seek immediate medical attention.
Weakness in the foot and numbness or pins and needles. There are times when clear weakness to the foot and toe muscles and altered sensation (numbness, pins and needles) can indicate that referral to the spinal surgeon, neurosurgeon or specialist orthopaedic consultant is required. In the past it was considered more of an emergency. We now recognise that most of the time the muscle strength and altered sensation do occur with sciatica, but heal.
Spinal Stenosis is a condition where the central spinal cord can be compressed and can sometimes be alleviated by Chiropractic treatment, but can also require surgery.
Lateral Canal Stenosis is where the nerve can be compressed exiting the spine. Sometimes this can be treated with Chiropractic and sometimes, once again, may require surgery.
Spondylolisthesis - when one of your back bones slips forward and out of position, possibly due to trauma in early life, or accident.
Tumours, infections, Osteoporosis and Cyst – These can affect the disc and the nerve.
Sciatica Prevention
The following can play a key role in protecting your back.
- Exercise Regularly
- Take breaks!
- Walk regularly, even if it’s just a few minutes, or longer if you are comfortable.
- Rest your back lying down some of the time
- Avoid heavy lifting
- Sit as little as possible. Some Chiropractors advise not sitting at all!
If you need or must sit or do computer work;
- Use a sit-stand desk so you can vary your working activity or position:
- Stand to work some of the time
- Use a ‘move-stool’ or similar high stool, to reduce the back angle
- Floating-tilt chairs are excellent for reducing the build-up of pressure on the sciatic nerve.
- Use a cordless headset to stand up and walk about whilst on the phone.