Ligaments are fibrous connective tissue that stabilize joints and prevent excessive movement both in rest and during normal movement. Ligament injuries are a very common cause of musculoskeletal joint pain and disability. They create imbalance in joint mobility stability, which can lead to wear and tear and osteoarthritis.
Ligament injuries can heal slowly. How long a joint, muscle or ligament will take to heal will depend on the severity of the injury and can take months or years. Often ligaments do not regain their full strength. I write about grades of injury and healing times in musculoskeletal injuries and healing times.
Severity of ligament injury is graded from one to three:
Grade 1: Stretching of the ligament or soft tissue stretch with no joint laxity or macroscopic tears
Grade 2: Some joint laxity with partial macroscopic tears
Grade 3: Excessive joint laxity and severe macroscopic tears (surgery may be required).
Incomplete ligament healing can result in ligament laxity, predisposing the joint to further injury and joint instability, which leads to chronic pain, diminished function and ultimately osteoarthritis of the affected joint.
Ligament Strain and Healing – In Depth
Ligaments are primarily composed of water, collagen, and various amino acids. When ligaments are strained, the proprioceptive nerves activate muscle contraction to protect and stabilize the joint after injury.
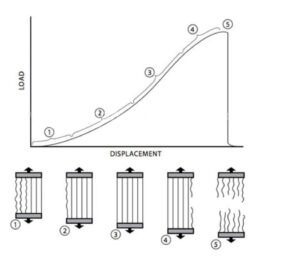
Stress on a ligament
Ligaments can become unstable, lax, loosen or lengthen when stretched or elongated past a certain point, or can tear under a high load.
LIGAMENT RESPONSE TO INJURY
Healing occurs in three phases:
The acute inflammatory phase
- Begins within in minutes of injury and continues over the next 48-72 hours.
- Blood collects at the site of injury.
- Platelet & fibroblast growth cells initiate clot formation with fibrin.
- Endothelial Growth Factor help new blood vessel to form, increasing vascularity in injured areas.
- Fibroblast Growth Factor promotes collagen and cartilage formation.
- Neutrophils, monocytes, and other immune cells ingest and remove debris and damaged cells.
The proliferative/repair phase
- Immune cells release various growth factors and cytokines.
- Fibroblast proliferation rebuilds ligament tissue.
- Scar tissue forms, but disorganised with more blood, fat, fibroblastic and inflammatory cells.
- Fibroblast cells deposit various types of collagen, proteoglycans, other proteins and glycoproteins.
- The collagen forms, but is abnormal and smaller than normal.
Remodeling phase – months to years
- The collagen and tissue matrix starts to resemble normal ligament tissue.
- The healed ligaments may look more like scar tissue.
- Ligaments heal but with laxity, are less pliable or elastic and may be weaker.
- Greater chance of osteoarthritis in joints.
Treatment to heal ligaments
Rest, mobilization, non-steroidal anti-inflammatory drugs, corticosteroid injections, and Prolotherapy, among others. While each of these therapies can help with the subjective symptom of pain following ligament injury, they do not all contribute to the cellular repair and healing of ligament tissue. In fact, some of these therapies have been shown to be detrimental to the ligament healing process by suppressing and inhibiting certain cellular processes that are required for ligament tissue repair. Other therapies have been shown to contribute to healing through their stimulation of certain cellular processes involved in the regeneration of ligament tissue.
Ligament Treatment – Movement NOT Rest
Early resumption of activity can stimulate repair and restoration of function, whereas prolonged rest may delay recovery and adversely affect the tissue repair. It has been shown that immobilizing a joint with a ligament injury can cause more scar tissue to form with a greater percentage of disorganized, weaker collagen.
Despite this, the old theory that rest or immobilization will prevent further tissue damage in the joint continues to prevail, and RICE (Rest, Ice, Compression, Elevation) protocol continues to be commonly prescribed as the first line treatment for ligament, tendon, and other soft tissue injuries.
Mobilization and exercise helps treat injured ligaments, joints and soft tissues
Early careful return to activity after injury has profound beneficial effects.
- Increased strength and collagen content of ligaments and tendons
- Mobilization forms more connective tissue, that is stronger and stiffer than if immobilized, and reduces scar tissue.
- Decreases muscle atrophy and helps prevent disuse osteoporosis
- Motion increases blood flow, providing nutrients and metabolites necessary for tissue repair.
- Repetitive loading helps ligaments and tendons detect strain and respond by modifying the tissue as it heals.
- Results of numerous animal studies have shown repaired ligaments are stronger if they are mobile, rather than at rest.
Studies show that patients who treated their ligament injuries with activity and movement, versus rest and immobilisation, experienced:
- That they were able to return to work and sports quicker
- They demonstrated less objective instability
- Movement decreased pain, swelling and stiffness
- They preserved a greater of range of motion
Steroid injections and nonsteroidal anti-inflammatory drugs (NSAIDs)
These can decrease inflammation and pain of ligament injuries for 6-8 weeks, but inhibit the histological, biochemical, and biomechanical ligament healing so are no longer recommended for chronic soft tissue (ligament) injuries and should be used for the shortest period of time, if at all.
Why are Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) detrimental to ligament, muscle and joint healing?
Prostaglandin-induced inflammation is required in an injury for the removal of necrotic debris and the initiation of the healing process.
NSAIDs specifically block the cyclooxygenase enzymes which catalyse the conversion of arachidonic acid to prostaglandins which play a significant role in ligament healing.
Furthermore, the analgesic effect of NSAIDs may permit patients to ignore early symptoms of ligament injury, further damaging ligaments, and thus delay definitive healing.
Studies showing NSAIDS inhibit ligament healing
One Australian study looked at the use of Piroxicam in the treatment of acute ankle sprains in the Australian military. While the recruits were able to resume training more rapidly, in the long-term, there was an increase in ankle instability. Multiple studies on the use of NSAIDs of the cyclooxygenase-2 (COX-2) inhibitor class have shown to inhibit ligament healing, leading to weakened mechanical strength.
- NSAID treatment is now used with caution for athletes with ligament injuries.
- NSAIDs are no longer recommended for chronic soft tissue (ligament) injuries,
- NSAIDs for acute ligament injuries should be used for the shortest period of time, if used at all.
Corticosteroid injections are strongly detrimental to ligament, muscle and joint healing
Steroid injections can decrease inflammation and pain of ligament injuries for up to 6-8 weeks but the histological, biochemical, and biomechanical healing of ligaments are inhibited.
Their anti-inflammatory actions prevent lysosomal enzyme release and inhibit essential neutrophil, cytokine and other inflammatory cell synthesis at the injury site. They inhibit fibroblast function and even cause collagen necrosis at the injection site. The steroid-injected ligaments are weaker. Because of these inhibitory effects on ligament healing, several extensive reviews have cautioned against their use to treat ligament injuries especially in athletes.
Platelet-Rich Plasma (PRP) therapy
Platelet-rich plasma therapy is a new treatment that aims to stimulate the natural growth factors your body uses to heal tissue. Plasma is fluid in the blood, mainly water and proteins, and helps red and white blood cells to circulate throughout the body, along with platelets or thrombocytes that help blood clot and play a key role in the body’s natural healing process.
Platelet-rich plasma (PRP) therapy injects a patient’s own platelets to speed up healing of injured muscles, ligaments, tendons, or joints. It aims to harness the patient’s own healing system. PRP is a centrifugal concentrate of the patient’s platelets, which are injected, sometimes using ultrasound guidance, to the exact site of injury. Studies show an improved inflammatory healing reaction involving fibroblastic and capillary proliferation, along with simulating fibroblast and platelet-derived growth factors, which help the soft tissue repair in muscles, tendons, and ligaments with acute, traumatic or overuse injuries.
Common uses for PRP
- Shoulder pain caused by rotator cuff tears
- Achilles tendon ruptures
- Tendonitis or chronic tendinosis such as tennis elbow or golfer’s elbow.
- Other soft-tissue injuries are becoming more common
Advantages of PRP
- Reduce or replace anti-inflammatories or stronger medications like opioids.
- Side effects of PRP therapy are small
- The body will not reject or react negatively to one’s own platelets
Conclusion
Ligament injuries are very common and can lead to joint instability and osteoarthritis if they do not heal properly. They create disruptions in the balance between joint mobility and stability, causing damage to the joint and other structures in and around it. Unhealed ligament injuries can ultimately lead to the most common joint disorder in the world: osteoarthritis.
Ligaments heal through a distinct sequence of cellular events that occur through three consecutive phases. The healing process is often slow and incomplete.
Numerous strategies have been employed over the years attempting to improve ligament healing after injury or surgery. One of the most important advances in the treatment of ligament injuries has come from the understanding that controlled early resumption of activity can stimulate repair and restoration of function, and that treatment of ligament injuries with prolonged rest may delay recovery and adversely affect the tissue to repair. Likewise, although steroid injections and nonsteroidal anti-inflammatory medications have been shown to be effective in decreasing inflammation and pain of ligament injuries for up to six to eight weeks, the histological, biochemical, and biomechanical properties of ligament healing are inhibited. For this reason their use is cautioned in athletes who have ligament injuries. As such, NSAIDs are no longer recommended for chronic soft tissue (ligament) injuries, and for acute ligament injuries should be used for the shortest period of time, if used at all. Regenerative medicine techniques, such as Prolotherapy, have shown success in case series involving ligament injuries of the spine and peripheral joints, but studies in more controlled settings and with large numbers are needed in the future. For more information, please see the Journal of Prolotherapy’s overview of ligament injury and healing.