Headaches are common: they affect 9 out of 10 of us.
As a chiropractor, I love treating headaches because many times they are caused by tension at the base of the skull, neck and spine and so they often respond so well to treatment. I firmly believe Chiropractic should be tried as one of the first treatment options, provided there are no headache ‘red-flags’ which can be ruled out in the history and examination.
Tension headaches
These are the most common, ‘normal’ everyday headaches, experienced by approximately 90% of adults at some point in their life. A tension headache may be described as a dull ache with constant pressure around the front, top and sides of the head as if a rubber band has been stretched around it. Commonly related to tightness in the neck, tension headaches are well treated with chiropractic.
Tension headache symptoms
Tension headaches can be related to stressful events, overworking, and tiredness. Stress, from work, daily-life and relationships is a very common headache trigger.
When we get stressed our adrenal glands release adrenalin which sensitises the pain receptor nerve endings in the body. In addition the central nervous system can become sensitised to on-going pain messages so that the pain persists even after the injury has gone. This is a plausible potential cause of tension headaches.
Psychological factors are also linked to tension headaches.
Cervicogenic or ‘Neck-Related’ Headaches
Headaches arising from the neck are very common and Chiropractic is an excellent treatment option.
Cervicogenic means ‘of neck origin’. Tightness or spasm in the neck can refer pain into the head, forehead, over the eyes or temples.
The headaches are often aggravated by certain postures or neck movements. A vice-like feeling around the head can be reported and the headache may ease when avoiding stressful neck positions or when lying down, as the neck muscles can relax with head supported.
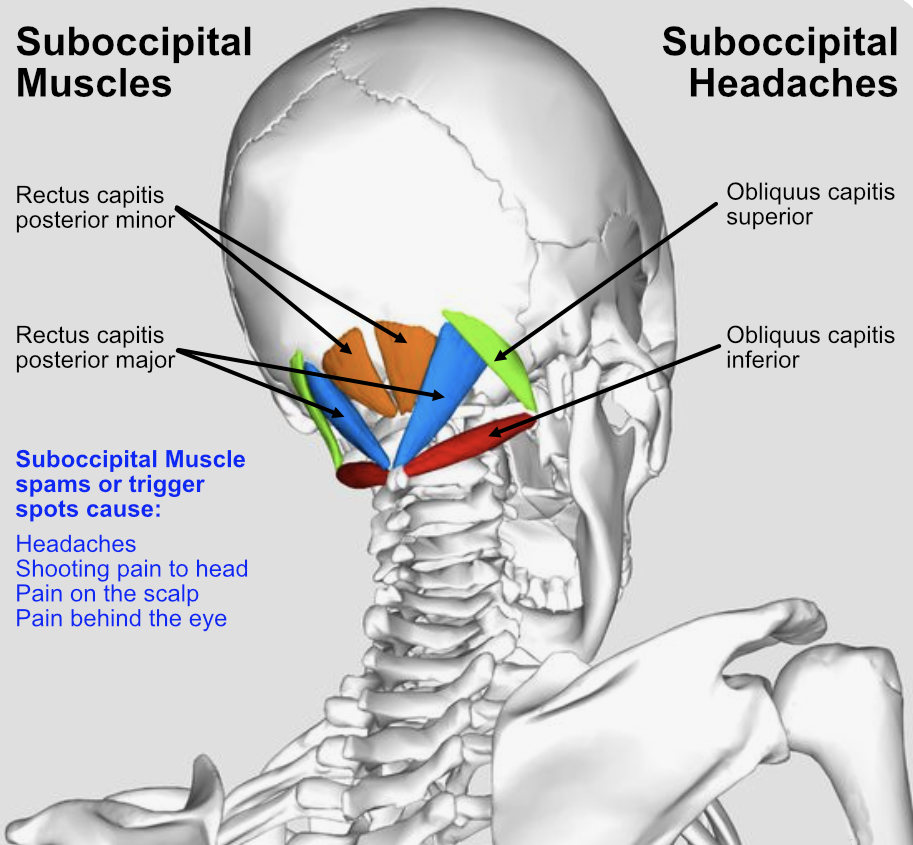
The head, which is quite heavy (5-6kg or 10-15lbs) rests and balances on the ‘Atlas’, the top vertebra at the base of the skull, along with a network of small postural muscles, called the sub-occipital muscles, and larger muscles attaching down the neck to the upper back. When these muscles are tight, or the vertebrae are fixed or not moving correctly, they can cause headaches.
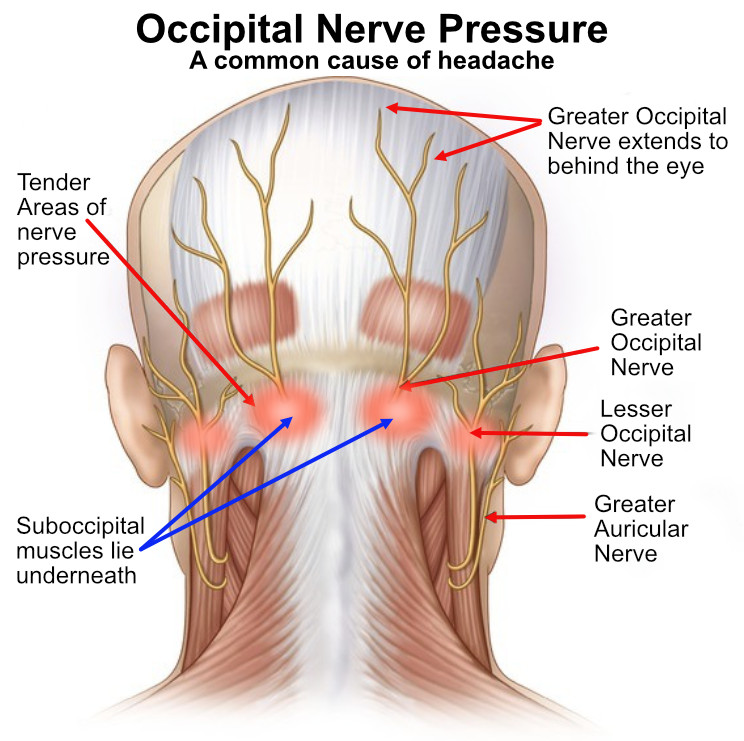
There are nerves underlying these deep neck muscles, that when irritated or pressured can cause pain up over the head and around to the back of the eyes.
Symptoms of cervicogenic headaches
Chiropractic Treatment of Headaches
Chiropractors are well trained in the treatment of headaches. Therefore chiropractic adjustments to the neck and upper back can be very effective not just to relieve symptoms, but also to cure the headaches in the long-term. Similarly, deep releasing muscle treatment to the upper spine and base of the skull, called the suboccipital muscles, gets to the root of the issue.
Personally I have found so many clients have been helped over the years and it gives me huge satisfaction when I can make a profound difference to their quality of life. As a chiropractor, apart from treatment, I will guide you into making some lifestyle changes that will prevent the problem from recurring. This could include:
Is chiropractic treatment effective for headaches?
My decorator client Martin is a fantastic example of how chiropractic treatment can help headaches. Martin has been my client for over 15 years. His work means that he is often extending his head back, looking up painting or papering ceilings, which brings on headaches. He suffers from tension at the back of the neck, sometimes with further symptoms of dizziness.
Treatment consists of deep massage to the base of the neck and suboccipital muscles and sometimes adjustment or manipulation of the cervical spine if the neck is particularly tight, or the symptoms are more severe. I give the manipulation after deep massage to help him relax fully. Sometimes I give only deep massage and the headaches settle. The combination of treatments is most effective at settling the headaches for a longer period of time.
Cervical headaches are commonly reproduced or triggered during treatment by pressing, even gently, into the neck muscles (especially suboccipital muscles at the top of the spine) which are often tender and this is a good sign the headaches are likely to respond well to treatment. There is often a stiffness or reduced movement in the neck, with pain sometimes radiating down into the arm or top of the spine in the Trapezius muscle area, an area which most clients call the shoulder, but is in fact closer to the spine or ribs.
Occipital Neuralgia (headaches caused by suboccipital nerve spasm)
Occipital Neuralgia is inflammation of the nerves that run up from the base of the skull, through the scalp and to the back of the eye. It is often caused by suboccipital muscle spasm or trigger spots which are just below the base of the skull or occiput at the top of the neck. It is a sensitive area with postural reflexes and sensory nerve endings lying beneath which can easily be pressured.
Anatomically, the greater and lesser occipital nerves arise from between the first and second cervical vertebrae. They have a thick covering and emerge from below the suboccipital triangle under the obliquus capitis inferior muscle and pass through the semispinalis muscle before rising to innervate the skin and scalp over the top of the head to behind the orbit.
Often times patients will point to the base of the skull and say ‘this is where I feel the tightness’. The pain can be described as migraine-like and, in fact, the symptoms are so similar that many patients believe they have migraines or cluster headaches when in actual fact they are suboccipital (neck tension) headaches.
Can chiropractic fix headaches
Tightness and pressure on the suboccipital muscles is a common cause of headaches.
Symptoms of occipital neuralgia
Lifestyle and work causes of cervicogenic headaches
Migraines
There is an overlap between migraines and headaches and an exact diagnosis is not always clear-cut.
Migraines are severe and intense headaches, usually on one side of the head, often described as pulsating, throbbing, perforating, pounding or debilitating. Other symptoms often present themselves, such as visual disturbances or sensitivity to light, nausea or vomiting, numbness, tingling and difficulty talking.
Migraines can start in childhood or early adult life, tend to affect women more, and can run in families. They affect about 1 in 6 people in the UK.
Neck and spinal tension can be a contributory factor to migraines and when this is the case, chiropractic has been shown to help in migraine treatment. Often when a migraine occurs it can stop you in your tracks and you are unable to work. It is important to get to the root of the issue and this is where my passion lies as a chiropractor.
Four stages of migraine
Stage 1
Migraine prodome
(early symptoms)
- Lasts a few hours or 1-2 days before. There are often mood changes, anxiety, depression, and/or euphoria; difficulty concentrating, tiredness, yawning, and difficulty sleeping.
- You may notice stiff muscles, especially in the neck, as well as nausea, increased urination or thirst, and unusual food cravings.
- During this phase it may be possible to reduce the severity or prevent a full a full-blown migraine, such as by taking medication early and avoiding or reducing the trigger factors. That could be avoiding specific foods or alcohol, and practicing relaxation or Alexander Technique to reduce stress both physically and mentally.
Stage 2
Migraine aura
One-third of migraine sufferers experience aura which build gradually and last 5-60 minutes, sometimes longer. You may experience:
- Blurred vision, seeing shapes, blind spots, bright spots or flashing/shimmering light, or loss of vision in one or both eyes.
- Headaches may occur before, during or after the aura, or not develop.
- Other symptoms include pins and needles, weakness or numbness in the face, on one side, or one arm or leg. Difficulty speaking, noise and light sensitivity. Lack of muscular control, perhaps with jerking movements.
Stage 3
Migraine attack
(the headache)
Migraine headaches usually last from several hours up to three days and range from being mild to debilitating.
- Pain can throb, pulse or change sides left or right (often starting one side and moving to the other), or be on both sides.
- Nausea, light, sound and smell sensitivity, with inability to sleep. Carrying out normal everyday activities can be very difficult during the attack phase.
During an attack, many people find sleeping or lying in a quiet darkened room can help.
Stage 4
Migraine post-drome
(the “hangover”)
This stage occurs in about 80% of migraines. The length of the phase can vary, or not occur at all.
Some migraine sufferers report the hangover or feeling washed out can be as debilitating as the headache.
Common symptoms include fatigue, muscle aches and joint pain, lack of concentration, dizziness and sensitivity to light.
Avoiding the triggers, relaxation activities, drinking water and avoiding stress can all help at this stage.
Why am I experiencing migraines? The potential causes of migraines
The exact cause of migraines is not fully understood. Migraines are considered to be a neurological condition, that triggers temporary changes in blood flow and chemicals like serotonin in the brain, that helps regulate pain in the nervous system and neurotransmitters such as calcitonin gene-related peptide (CGRP). The brainstem and the trigeminal nerve may also be involved.
Migraines generally peak during your 30s, and gradually become less severe and less frequent in the following decades.
Some people find migraine attacks are associated with certain triggers, which can include:
- Stress and tiredness, along with emotional anxiety
- Sleep changes – not enough or too much sleep, or altered sleep routines, like travelling or jet lag
Hormonal changes in women causing migraines
Women are three times more likely to have migraines, often occurring shortly after onset of menstruation with oestrogen fluctuations. Pregnancy may alter the frequency, and generally migraines improve after menopause.
Oral hormonal contraceptives and HRT (hormone replacement therapy) can affect migraines.
Nutritional factors – foods that contribute to migraines
The four classic ‘C’s that can cause migraines are Cheese, Coffee, Citrus and Chocolate.
Other foods that may contribute to migraines include:
Other causes of migraines
Treatment for Migraines. What options do I have?
Medical treatment for migraines
These include over-the-counter painkillers like paracetamol and ibuprofen or Triptans – medicines that can help reverse the changes in the brain that may cause migraines. High blood pressure medication can be prescribed.
Amitriptyline and tricyclic antidepressants have been used, or Nortriptyline. If you have nausea or vomiting, your doctor may suggest anti-nausea or antiemetic drugs.
Alternative or complementary approaches for helping migraines
There are many alternative treatments and lifestyle changes that can all help reduce your migraines. For many migraine sufferers the medication over the counter or prescribed by their doctors do not help significantly and do have side-effects. They may help reduce symptoms if they are taken early enough, but many clients look for more effective, safer, long-term treatment. In this case, chiropractic may be very helpful. To find out if chiropractic is for you, see What is Chiropractic or hear other patients’ experiences here.
Healthy Lifestyle changes to help Migraine
Regular exercise, reduced stress, relaxation, mindfulness relaxing activities can all help.
Getting regular sleep and eating regularly, staying well hydrated and reducing coffee and alcohol.
Yoga, Pilates, Alexander Technique, Acupuncture, Massage or Acupressure, Reflexology and mindfulness can all help general stress and tension and for some, this may cure or greatly reduce the severity of the migraines.
Seeing a nutritionist for diet coaching is a very sensible idea to help tackle any nutritional links or triggers for migraine.
Cluster headaches
Cluster or ‘alarm-clock’ headaches are a rare type of primary headache affecting about 1% of the population, 85% of them male. The pain is extremely severe but the attack is brief; it may be only a few minutes, or last an hour or two.
These excruciatingly painful headaches cause an intense pain around one eye, which can be inflamed or watery, with possible nasal congestion. They’re rare and are called cluster headaches because they happen in clusters for a period of time, commonly lasting weeks or a month or two at a time around the same time of year.
They can strike in the middle of the night, or often at the same time each day. A history of heavy smoking and drinking is common, and alcohol can trigger attacks.
Pharmacy medications don’t ease the symptoms of a cluster headache, but a doctor can prescribe specific treatments to ease the pain. Chiropractic treatment is worth a try!
Primary vs secondary headaches: what is the difference?
About 90% of headaches can be classified as primary headaches, that aren’t due to another underlying health problem.
There are many types and classifications of primary headaches, commonly:
- Tension headaches commonly caused by tight muscles and stress
- Cervicogenic headaches related to neck or spinal injuries
- Migraine headaches
- Cluster headaches
About 10% of headaches can be classified as secondary headaches. These are caused by an underlying medical condition, medication, or drugs. Another common cause is a hangover!
If you’re suffering from bad headaches it’s natural to think something serious may be wrong, but headaches from a serious medical condition, such as infection or increased pressure in the skull due to a tumour, are very rare. Listed below are some, but not all, of the secondary causes of headache:
- Colds, sinusitis, flu, allergic or immune reactions can tend to cause a generalized joint inflammation, which can also increase muscular spasm where tension is underlying. The headaches can be triggered or ‘spontaneously arise’ due to these illnesses, which can persist and worsen, even after the initial illness has subsided.
- Medication overuse can cause headaches, even overuse of medications intended to treat headaches themselves! Stopping the medication can help, but should be done under the advice of your doctor.
- Hormonal headaches in women, often linked to the menstrual cycle, along with the pill, menopause and pregnancy.
Medications previously considered “safe” can be common causes (called analgesic rebound headache, medication misuse headache or drug-induced headache). Among the list are:
- Nonsteroidal anti-inflammatory drugs (or NSAIDs, such as ibuprofen and naproxen)
- Sinus relief medications
- Acetaminophen
- Sedatives for sleep
- Codeine and prescription narcotics
- Over-the-counter headache remedies with caffeine such as Anacin, Excedrin and others. Excess Excedrin can trigger serious medication-overuse headaches
- Opiates
- Vasodilators, such as nitroglycerin
- Excess Aspirin
Medication-overuse headaches start when medications stop relieving pain but start to cause headaches. This can prompt you to want to take more pain medication, which creates a negative cycle.
Headache Prevention Tips
- Avoid getting locked in one position for too long! Take breaks every 30-60 minutes, especially with computers, tablets and phones where we can all too easily look down too long (see Text neck and Chiropractic) or other activities like ironing, using a sewing machine, working on an addictive puzzle or reading.
- Gentle, relaxed movement or exercise, where you can avoid strain to the neck, may help relieve the pain associated with primary headaches. Be cautious of heavy or high-intensity exercise.
- Clenching the teeth can also contribute to headaches. Temporomandibular joint (TMJ) dysfunction is a link. This can be helped with Chiropractic or Alexander Technique.
- Keep Hydrated! Sip water regularly to avoid dehydration, which can lead to headaches.
Migraine & Headache Red Flags: When to See a Doctor
Headache ‘red-flag’ signs & symptoms that require urgent medical attention:
- Trauma, accident or injury with a head-blow. You may experience a progressive continual headache after. This is a red flag, especially if it is slowly getting worse and not settling.
- Sudden onset headache that is excruciating, constant and worsening, with possible neurological signs including altered mental status and loss of consciousness.
- An abrupt, extremely severe headache, called ‘thunderclap headaches’.
- Headache with fever, stiff neck, mental confusion, seizures, double vision, weakness, numbness, trouble speaking or vomiting.
- A chronic headache that is worse after coughing, exertion, straining or a sudden movement.
- Meningitis – you are generally unwell with a progressive headache, usually generalised or frontal, which worsens over a period of hours, sometimes accompanied by a stiff neck or nausea.
- New headache pain after age 50.

