You may have heard the term ‘referred pain’ before, but are not sure exactly what it means.
Simply put, referred pain is the pain from an injury which is felt in another part of the body, not the part of the original injury. For example, hip wear and tear causes pain in the knee or a heart attack can refer pain to the jaw, teeth, then shoulder and arm. We still don’t fully understand how this works, whilst there are several theories.
Local, distal or distant pain
It is useful to make the distinction between these terms:
Local pain is pain felt near the injury or origin; for example, palpating a muscle in spasm near an injury can be very tense and painful.
Distal means ‘situated away from the centre of the body or from the point of attachment’, so distal or distant pain is another term for pain away from the injury, origin or cause.
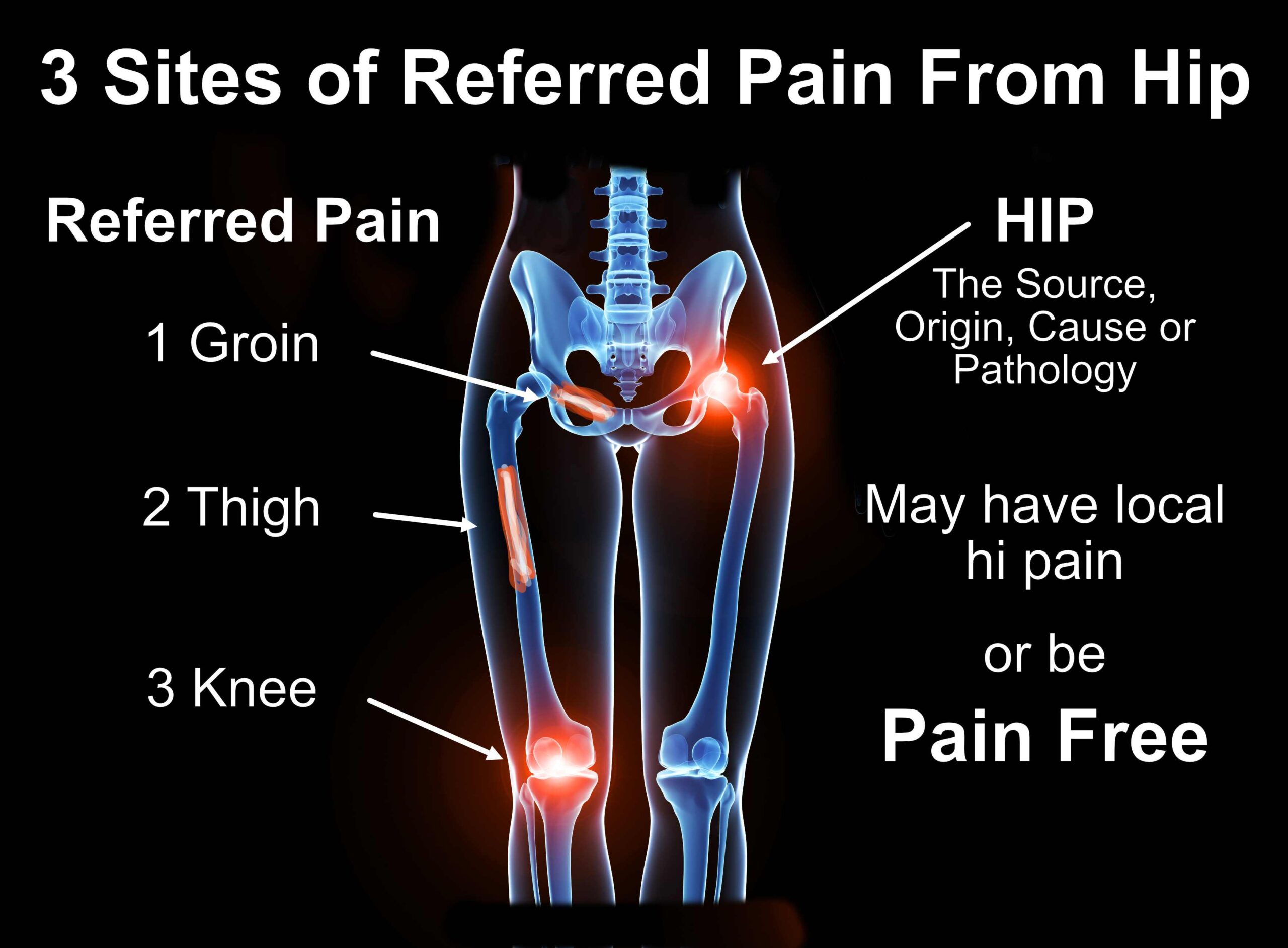
With hip arthritis, for example, three possible sites of referred pain are the knee, thigh or groin. There may be no pain at all in the hip, but, for example, just knee pain on walking.
Pain locally, referred or both
With some musculoskeletal conditions there can be local pain at the site of origin, or both local pain and referred pain, or even only referred pain.
Referred pain can mislead diagnosis and treatment
Referred pain can cause patients to be unsure about the origin of their pathology. They are in pain but just can’t figure out why. Health professionals can also sometimes be misled, especially if there is no pain at the site in the body causing the referred pain. It’s where good examination of the painful area and also investigation into the possible referral causes are essential.
Referred pain is a term also used when there is no clear pain down the path of a nerve (radiculopathy), such in pain down the leg in Sciatica, or in Brachial neuralgia down the arm.
What causes referred pain?
The cause of referred pain is not fully understood and there are many theories of why an injury in one area of the body gives you the experience of pain in another area. It happens because the nerves in your body are all connected. I learnt this from my neuroanatomy teacher at university when I was despairing about learning all the nerve paths and names. The way he described it to me was that ‘everything is connected to everything’.
Crossed-wires theory of referred pain
My favourite simple explanation is that an injury sends ‘nociceptive’ signals to the brain that there is a problem, but whilst travelling to the brain, these signals get ‘crossed’ with sensory signals from another area of the body, so the brain then ‘refers’ the pain signals elsewhere. There are many more detailed and complicated pain theories for referred pain.
Common examples of referred pain
Referred pain can be felt anywhere, especially in children, which can make diagnosis difficult. Common areas that are affected by referred pain include:
- Pain in the neck, left shoulder and arm (occasionally right) caused by cardiac ischemia.
- Brain freeze after eating ice cream or an iced slushy is also considered a type of referred pain. The cold ice stimulates the vagus nerve sending pain to the head.
- Pain in the shoulders from an injured spleen or liver cyst (also known as Kehr’s sign).
- Pain on the sides of the back can indicate kidney or colon pathology.
- Pain in the teeth and jaws can be an early symptom of a heart attack.
- Pain between the shoulder blades can indicate a stomach condition.
- Phantom limb pain. It has been known for amputees to feel pain from where the limb used to be, because part of the brain still thinks the limb is there. Not only that, but the amputated limb may cause referred pain elsewhere – for example, an amputated foot might cause referred pain in the upper thigh.
Common Musculoskeletal Pain referral patterns
- Knee, groin or thigh pain caused by hip wear and tear
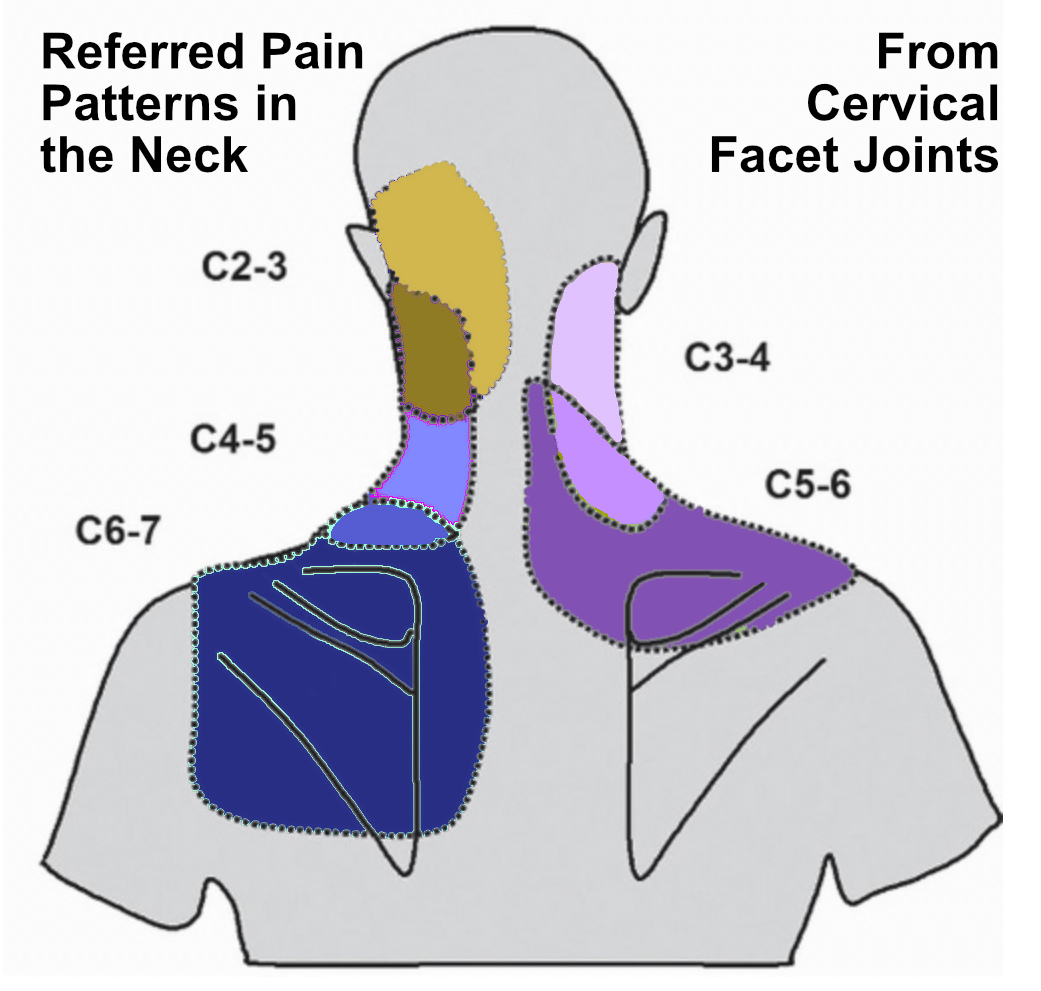
- Pain in the shoulder and upper back from the neck (see diagram)
- Sacroiliac joint pain into the groin or upper posterior thigh
- Headaches from the neck and suboccipital muscles
When to see a healthcare provider
If you’re having pain that is not settling, or severe and acute, even if there is not visible injury at the site of the pain, then it’s a sign to seek help.
Don’t wait for the pain to make sense or for the painful sensation to go away!
Treatment for referred pain
In most cases, Chiropractors and health care professionals needs to evaluate and treat the cause of the referred pain. If we treat the part of your body that’s in pain instead of treating the part that’s injured, the pain won’t settle. It’s so common when I treat that clients are continually surprised that I find tender muscles and joints on the opposite side to the pain, and they say ‘I didn’t know I had a pain that side’. The non-painful side can often be the more tender side, when massaged or palpated.
Trigger spots
These are painful or tight spots or ‘knots’ in muscles which cause pain, either locally or in another area of the body. Also described as ‘a small hypersensitive region from which impulses bombard the central nervous system and give rise to referred pain’. There are various uses of the term trigger point therapy or treatment.
Doorbell sign
This is a good sign of referred, or radicular, pain to another distal area of the body. It’s given the name ‘doorbell’ because there is an almost instant result of pain, which ‘rings’ in another area, like pressing a doorbell.
Common areas of doorbell signs are:
- Pressing on the base of the neck, the suboccipital muscles, causes headaches
- Pressing on a cervical facet joint refers pain to upper back
- Pressing on an injured nerve root in the neck simulates pain down the arm.
- Pressing on the piriformis muscle refers sciatic pain down the leg.
Often, when a doorbell sign is found it is an extremely helpful test in understanding the exact cause of the pain. Often clients say to me ‘That’s exactly the pain I get’ as I push on the ‘doorbell’ or cause of the pain. It’s very common, then, that with treatment holding the spot, massage and releasing techniques, the tight muscle causing the pain relaxes and the ‘ringing’ pain subsides, allowing the injury to heal.